Failure to tackle drug-resistant infections will lead to at least 10 million extra deaths a year, (largely exceeding the 8.2 million deaths/year from cancer, 1,5 million from diabetes 1.2 million from car accidents) and it will cost the global economy up to $100tn by 2050.
The Economist, Review on Antimicrobial Resistance directed by Lord O’Neill
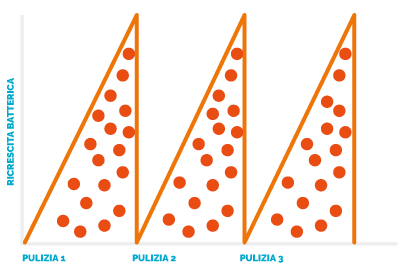
RESULT OF A CLEANING ROUTINE
WITHOUT BIOVITAE®
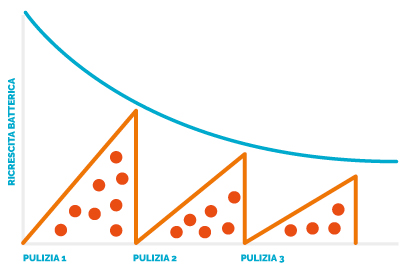
RESULT OF A CLEANING ROUTINE
WITH BIOVITAE®
ANTIMICROBIAL RESISTANCE
The abuse and misuse of drugs has triggered a global emergency because bacteria, through a series of mutations, have become drug-resistant, forming new strains (super bugs) that are increasingly stronger and resistant to antibiotics. To challenge what has been called “the greatest threat to modern medicine”, the World Health Organization (WHO) has issued a Global Action Plan highlighting the need to tackle infections through prevention rather than researching new antibiotics, because at some point they would however become ineffective, and prevention is the only weapon that will keep the existing molecules effective.
WHAT IS ANTIBIOTIC RESISTANCE
Antibiotic resistance is the ability of bacteria to remain indifferent to the action of an antibiotic. It can be intrinsic, when the micro-organism has never been affected by a particular antibiotic, or acquired, when bacterial strains that were previously sensitive to a specific antibiotic develop resistance against it.
HOW IT DEVELOPS
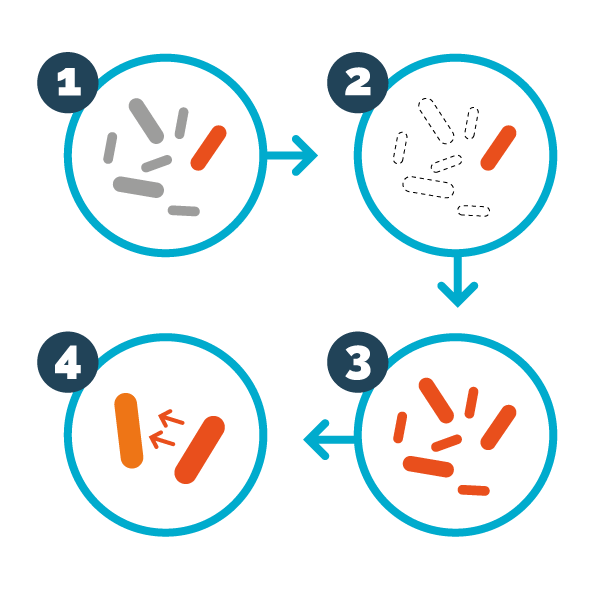
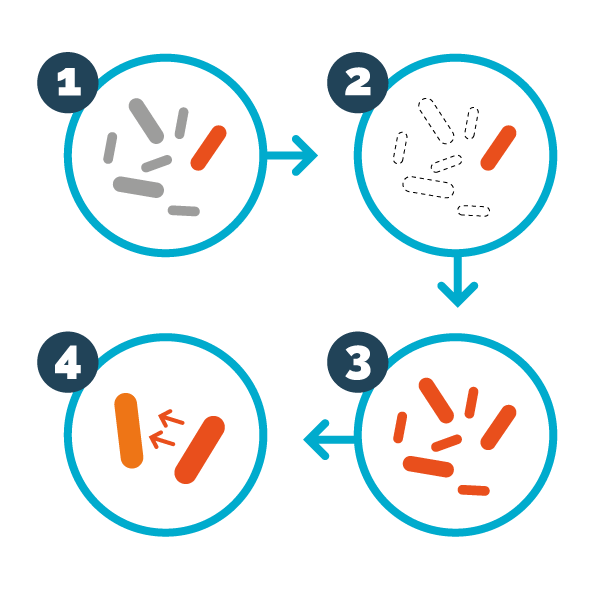
The development of antibiotic resistance is a normal evolutionary process. In a bacterial colony can live both sensitive bacteria and bacteria resistant to one or more antibiotics; and when an antibiotic kills the sensitive bacteria, those resistant to the drug, which until then were in a “dormant” state, begin to multiply, creating generations of resistant bacteria. And, as if that were not enough, resistant bacteria can transmit resistance to the antibiotic to every other microorganism that join the colony.
HOW BACTERIA PROTECT THEMSELVES
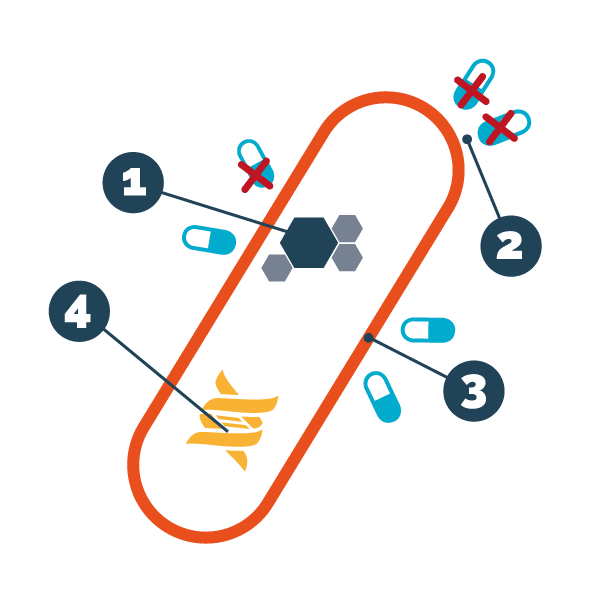
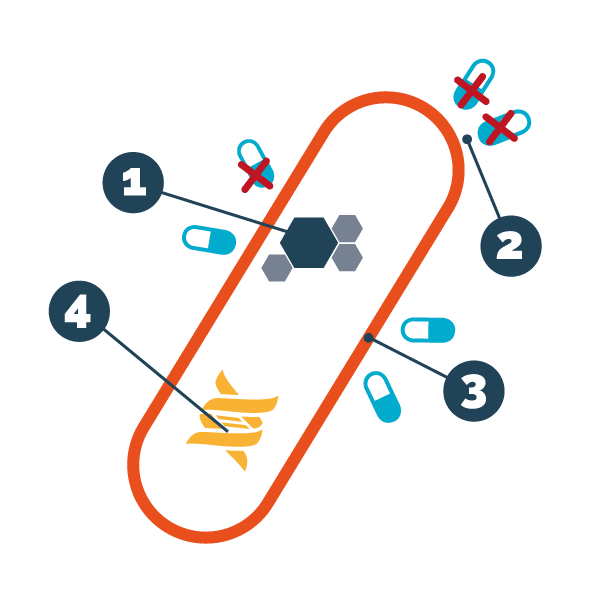
The acquired resistance is possible because the bacteria are able to modify their genetic heritage, both through spontaneous mutations and through the exchange of genes between different strains. Microorganisms have different alternatives to avoid the lethal action of antibiotics, namely: 1. production of enzymes that inactivate antibiotics; 2. rapid elimination of the antibiotic; 3. waterproofing of the bacterial wall to the antibiotic; 4. alteration of the target of the antibiotic.
THE HUMAN BEHAVIOURS THAT PROMOTE RESISTANCE TO ANTIBIOTICS


1. the incorrect use of antibiotics, also to treat viral infections where they have no use; 2. taking antibiotics differently from the prescriptions, i.e. at lower doses or for a different time period than recommended; 3. the habit, not always justified, of administering antibiotics for preventive purposes.
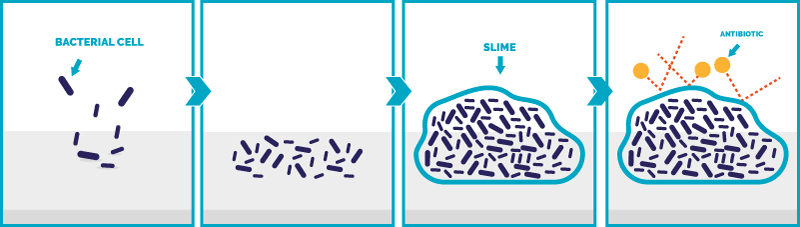
THE BACTERIAL BIOFILM
The main cause of bacteria becoming resistant to antibiotics is the BACTERIAL BIOFILM, a compact mass of filaments (pili), sugars and proteins that forms on the surfaces, in which the colonies of bacteria are able to grow and exchange information, becoming resistant. The biofilm is the most impermeable liquid substance ever discovered, which masterfully isolates the bacteria from the action of disinfectants or antibiotics. Because only light can go through the bacterial biofilm, the patented frequencies of BIOVITAE® are the only ones that can pass the biofilm and make it ineffective, killing bacteria inside it.